Hampshire Hospitals NHS Trust
To improve our knowledge about the wider needs of 10 patients with Epilepsy under the care of the BNHH paediatric epilepsy team by April 2023.
 |
 |
Project aim
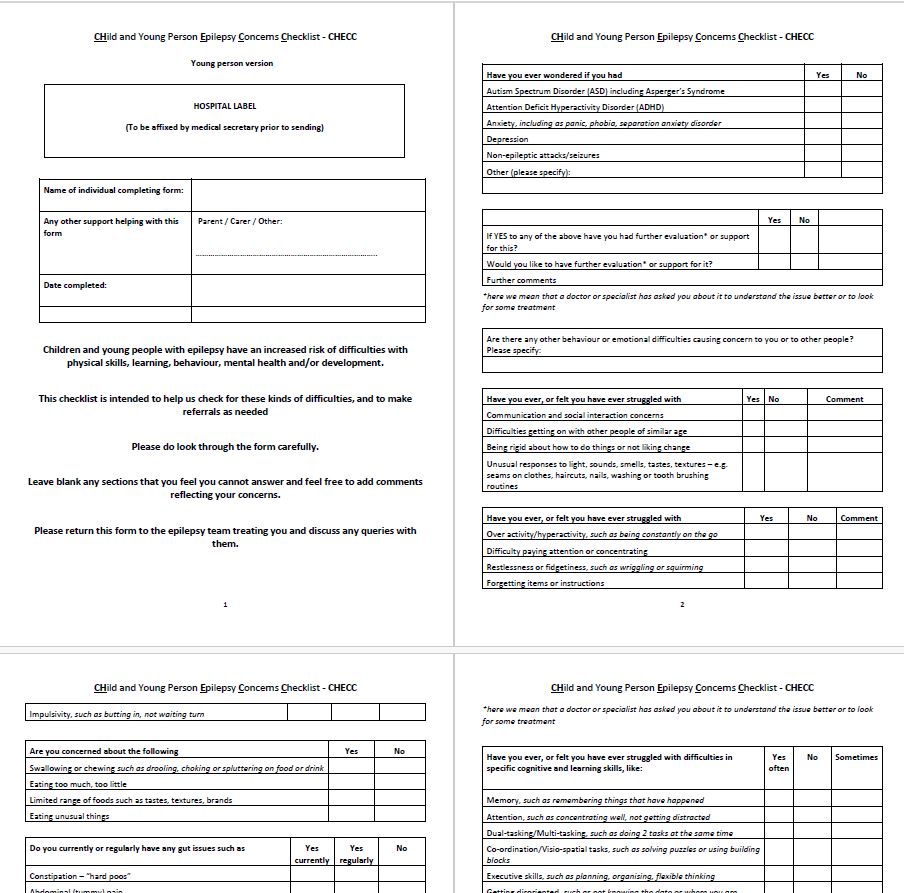
To better understand the wider educational and psychological needs of children and young people with epilepsy (cypwe) under the care of BNHH by piloting a measure to capture this, called the CHECC.
To improve our knowledge about the wider needs of 10 patients with Epilepsy under the care of the BNHH paediatric epilepsy team by April 2023.
Spread good and newly developed practice from one hospital to the other hospital in the Trust.
Background
We support a multidisciplinary epilepsy service comprising epilepsy paediatricians with epilepsy and paediatric Neurology /Neurodisability/neurodevelopmental expertise, epilepsy nurse specialists and highly skilled clinical psychologist. We work within an integrated care child health department including neonatal, general, community/paediatric neurodisabilty services, medical and nursing teams including special school nursing.
We have outreach joint paed neurology clinics from our tertiary centre in Southamptn. have the skills to identify, evaluate, support or signpost to CAMHS re additional mental health needs and neurodevelopmental conditions such as LD or ASD. We have adult epilepsy nurses to support cyp in transition and developing our transition pathways.
We undertake quality improvement interventions through epilepsy nurse activity, including school emergency training.
Creating and developing a Child and young person epilepsy concerns checklist (CHECC), info gathering carers, CYP and schools.
Project planning
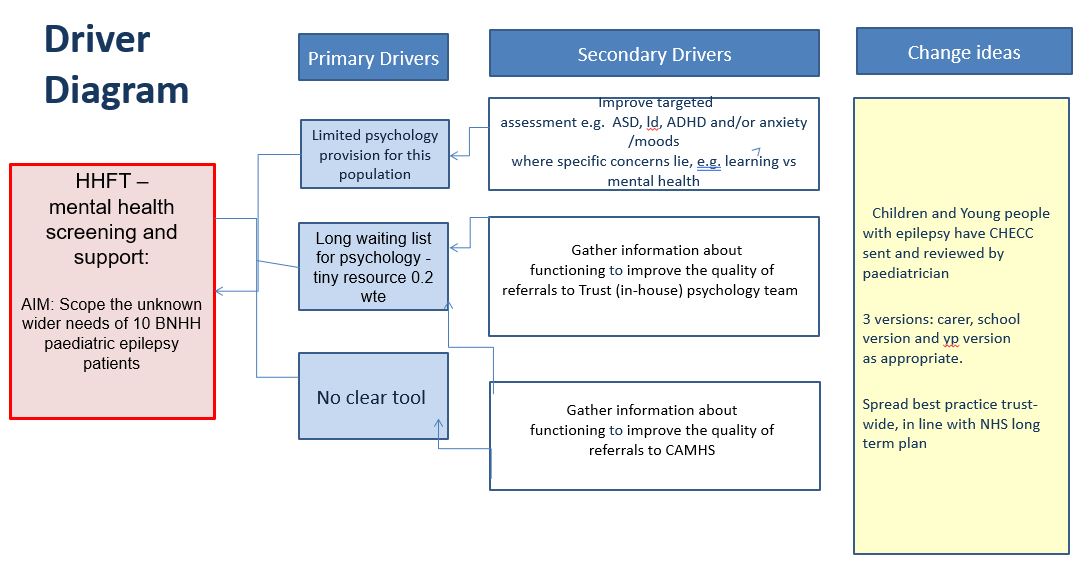
This project was chosen to develop our Hampshire Hospitals NHS Trust epilepsy service across two DGH hospital sites because the Trust has a different service provided re different historical funding patterns.
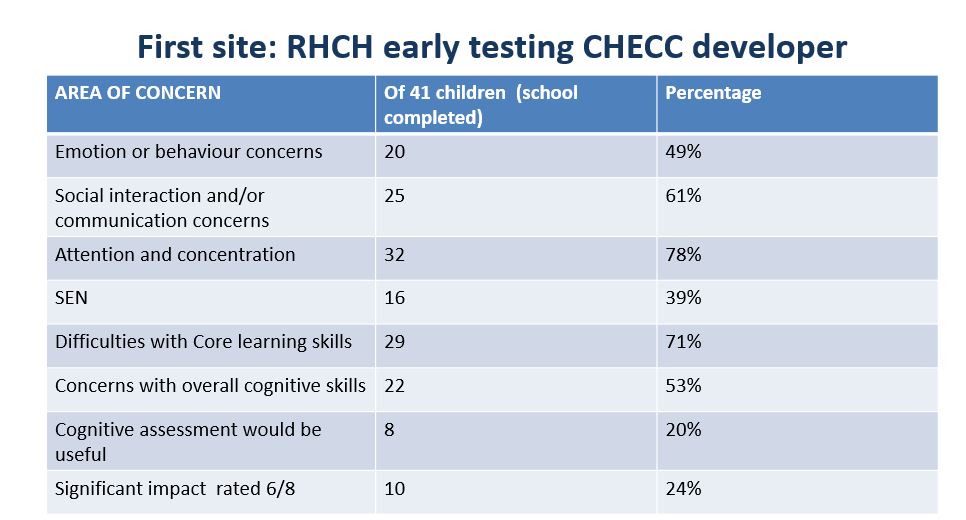
Royal Hampshire County Hospital (RHCH) had begun trailing the use of this measure to help provide better care to our epilepsy patients. In RHCH have some psychology input 0.2 WTE for assessment of children with epilepsy (including cognitive assessments) Basingstoke and North Hampshire Hospital (BNHH) does not.
We have regular HHFT epilepsy service meetings where we discussed the enhanced service at RHCH and decided as a team it was important to begin to replicate the work being done at RHCH to BNHH. Team part of Epilepsy 12 audit- enhanced service by introducing an epilepsy nurse to HHFT for BNHH in 2019.
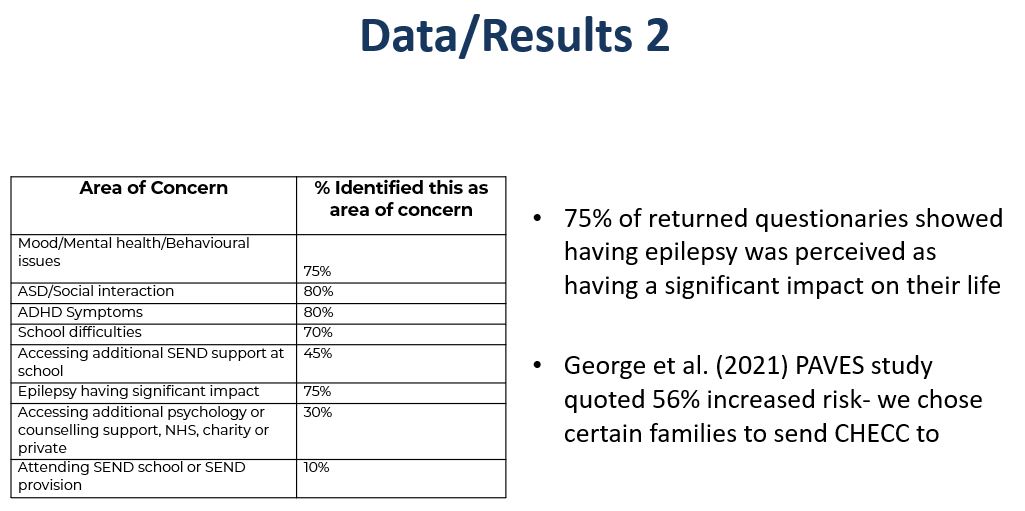
To capture the needs of the BNHH cypwe whose needs were unknown/uncaptured. CYPwE have significantly increased risk of developing emotional, learning, mental health and behavioural difficulties, compared to their peers and other children with chronic health conditions.
The first pathway is for patients that need support with psychological distress who are referred to general paediatrics psychology. The second pathway is for patients that have complex needs and having more difficulties in terms of learning or neurodevelopmental difficulties and referred to the Trusts neuro-disability consultant twice a month where children are jointly seen together.
The care provided includes follow-up assessments, monitoring of medications and physical check-ups. The pathways within Basingstoke does not exist in the same format for their patients. The psychology team discusses the referrals with the consultant that has completed the form with the family, then appropriately refers the child to the psychology service for support where they would decide on the best pathway to address the needs of the patient.
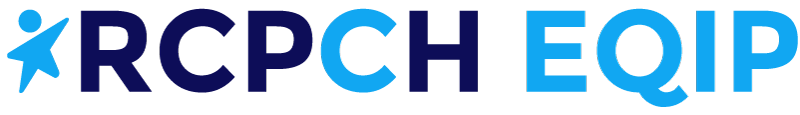
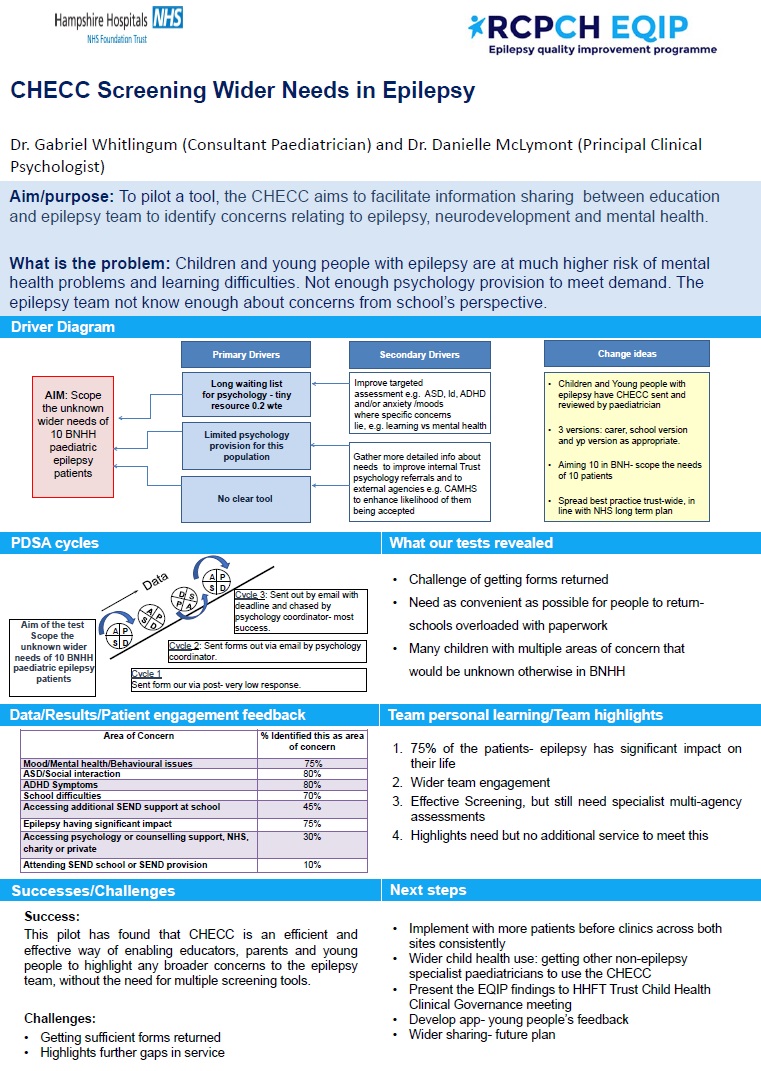
We used a driver diagram to help us focus on where the problems lay. Patients and families were involved in the development phases of the tool and asked if the measure was helpful, and for example, if it was too long or complicated to complete and revisions made. We will test a questionnaire on ten children which will work as a screening tool to determine the patients that should be referred for therapeutic support or those that require advance support from CAMHS due to complex needs that go beyond the remit of the psychology team.
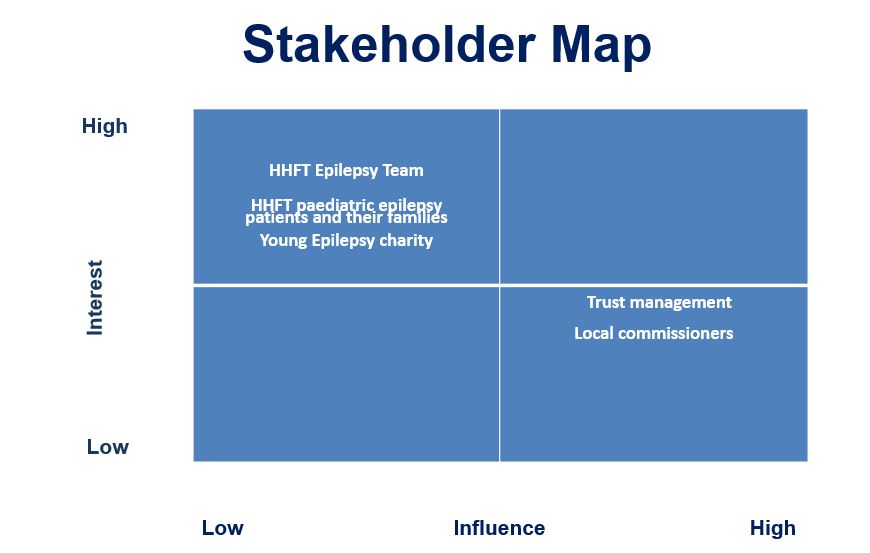
Tests, changes and what was learned in the process
November 2022
Using the CHECC won’t give us more psychology time. Current offer: Currently, you can make a referral to the paeds psychology team for support with emotional difficulties attached to being a child/young person with epilepsy or to one of the neurodisability clinics for (ASD + assessment).
So what are we hoping we’ll add by using the CHECC?
Understand their needs better and support them better. We could agree that for each CHECC you complete, we have a conversation about; How you can support them. When referral appropriate to paeds psychology or when a referral should be made to CAMHS, psychology giving you some resources/strategies around a specific area.
Next steps
In terms of admin, look at completed CHECCs sent and complete an audit of what it shows.
January/March 2023
It has been difficult for our cross-site team to engage children and young people in collating feedback on or sending back the questionnaire, therefore the team have liaised with epilepsy charity Young Epilepsy to support them in this task. Young Epilepsy will create a working group with their children and young people epilepsy cohort.
Examples of what we have learnt about their project since joining the EQIP has been getting a better sense of how many children within the service need additional support and the ability to scope who these children are and what their needs are.
A business case has been submitted to their commissioners that includes documentation on the needs of this group of children and how much more psychology time is required to support them. Additionally, the tool has provided more involvement from school and highlights important info on issues that would not have necessarily been uncovered, providing a more holistic approach to the care of the child rather than just being focused on the medical. Experiencing a broader perspective of the child and the dynamics within the family as well as in the school.
Patient engagement
- We engaged a variety of sources in this project, namely,; parents, and the Young Epilepsy Charity who liaised with their connected group of young people. We are also looking to develop the tool as an app- to appeal more to young people then a paper form.
- At the end of each checklist we asked them for feedback on us using this measure in clinic, with questions such as whether this 6-page form was too long, too short or about right. There were a wide range of responses. As a team we felt it was an okay length to be used, given the spread of responses.
- Other feedback was that it was helpful to highlight concerns that schools and some families held.
- All of the 12 respondents who gave feedback on education CHECC, indicated that it was potentially helpful.. 2 were unclear – though this was an earlier version of the checklist
- After seeking families and school’s views on the measure, we revised the questions.
- Planning to develop an app for the next stage of the project in connection with Young Epilepsy charity.
Methods:
- The CHECC measure was developed with input from parents, epilepsy charities and professionals including paediatric neurologist, neuropsychiatrist, psychologist, epilepsy nurse, general and neurodisability paediatrician.
- Three different versions of the checklist were created (parent/carer, education and young person version).
- Different questions were included in each version. All checklists had a specific space to set their top three goals.
Results
November 2022/January 2023
Round 1 Pilot in BNHH: CHECC Forms sent to the families of 21 patients. School/nursery, parents’ version and self-report versions. Outcome: Forms received regarding 12 patients, a 57% response rate.
Respondents:
- 30% from parents
- 40% from schools
- 30% from young people
March/May 2023
- Despite people presenting in clinic with concerns, that contacting them “cold” with a form to complete does not get us the information sought. This did not work. In the original RHCH pilot, the form was mentioned in a clinic and this got much better response- 41 patients responded.
- Abandoned sending it cold in the post, needed to email it and chase people- more proactive.
- Feedback from the forms suggested sending it before the clinic would be of most benefit.
- Feedback was also to make it digital- next step via Young Epilepsy.
- Ideally would upload to EPR- electronic patient record so Paediatrician can review before brining into the clinic room, or whilst they are there.
- We’ve learned about the challenges of changing practice of clinicians particularly at times of great challenge and trust under increasing financial scrutiny.
- Usefulness of having one form to send people to capture concerns.
- We’re beginning to scope the size of the unmet need within our trust, where two trusts became one, but years later there’s still huge differences in service provision.
- We’ve been harmonising service delivery across both hospital teams and sites, but still more improvement is needed.
Challenges
- The main issue with mental health and neurodevelopmental assessments is they are very time consuming and there’s a lengthy waiting list.
- Patient engagement has been difficult in getting their involvement. The team have sent out the questionnaires via postal methods. 10 families have been sent the questionnaire and one so far has been received back.
- The team have also experienced difficulties with school involvement with questionnaire because they often have fedback they haven’t received it.
- The lack of admin to support the team to evaluate questionnaire results has also been a challenge.
- Hospital pressures are increasing due to winter pressures, so capacity is low in terms of staff resources is low unable to meet regularly.
- Cross-site team so have not yet found a way to effectively communicate together as a team.
- Lack of patient feedback to fill in the questionnaire used as a screening tool.
- Initial attempts to get data were completely unsuccessful.
- Very difficult to bring together the whole team to make a team effort.
- The team member’s timelines didn’t work out, e.g. having trainee support
- In reality was difficult to implement this change within the team who wanted more understanding of the patient group.
What we would have done differently:
- Brought more epilepsy-focused admin staff in sooner.
- Financially- business case not yet supported, wanting more psychology and SLT- ASD assessment
Successes
- We achieved the project aim and scoped wider needs of 12 children/young people.
- Paediatrician will have information to draw on to discuss with the family at the next appointment including information from education, which previously would not have been available.
Next steps
- Discuss EQIP outcome at next epilepsy service meeting.
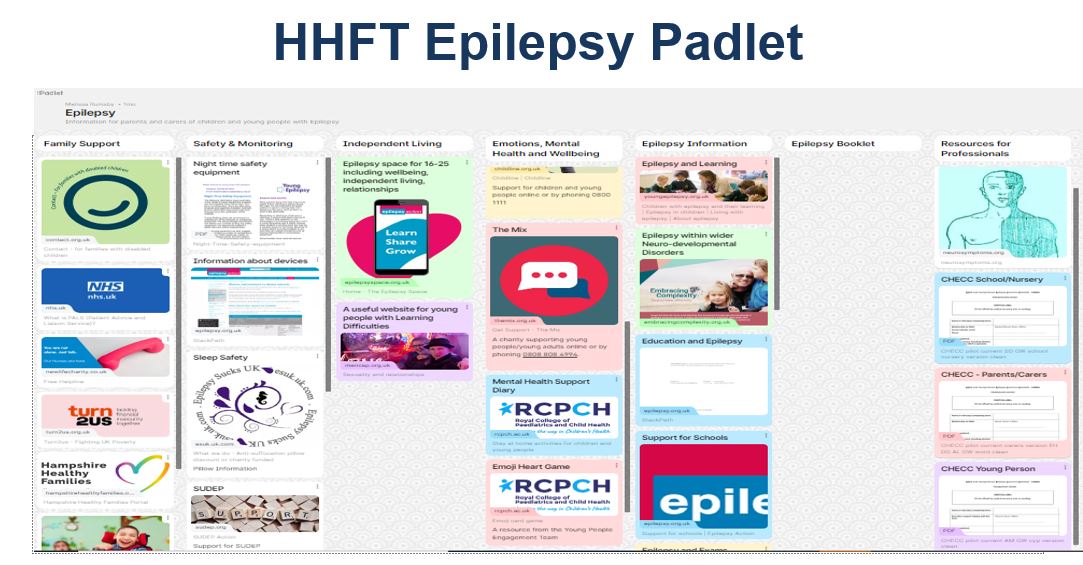
- Develop Padlet further- more self-help resources, e.g. anxiety, anger, low mood.
- Wider Child Health: Present at Child HHFT Health clinical governance meeting and introduce the measure to be used by non epilepsy specific paediatricians who may see epilepsy patients too- big challenge.
- Develop the app- most appeal to young people and more efficient way of getting the information into the paediatrician’s hand in clinic. More environmentally and young-people friendly.
- Have form on a device in waiting room
Hampshire Hospitals NHS Trust team presentation and project poster
Download to view Hampshire Hospitals NHS Trust team project presentation slides and poster including examples of CHECC questionnaires
Team presentation project slides (696.2KB) Team project poster (161.7KB pdf) CHECC 1 Young person version (221.6KB pdf) CHECC Parent/Carers version (266.1KB pdf) CHECC 1 School/nursery version (266.1KB pdf)Additional resources available to in relation to the work completed for CHECC
Additional resources available to view and download in relation to the work completed prior to EQIP
Poster presented at BACCH event (110.5KB) Slides presented at BACCH event (5.2MB) Abstract submitted for 15th European Paediatric Neurology Society Congress (49.9KB pdf) CHECC Child and Young person Epilepsy Concerns Checklist. A holistic epilepsy and wider needs surveillance tool, BPNA (181.1KB pdf)