The Dudley Group NHS Foundation Trust
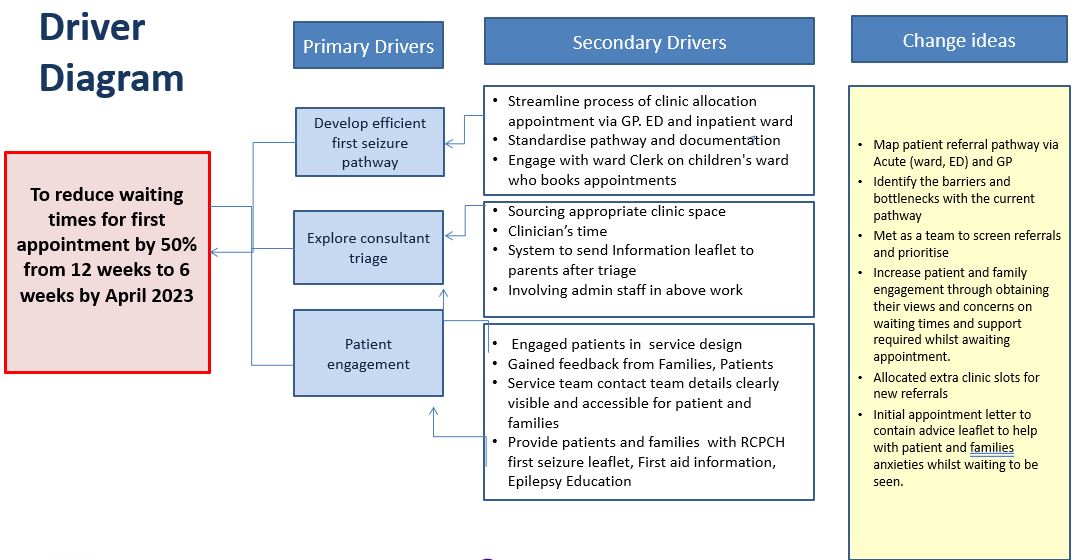
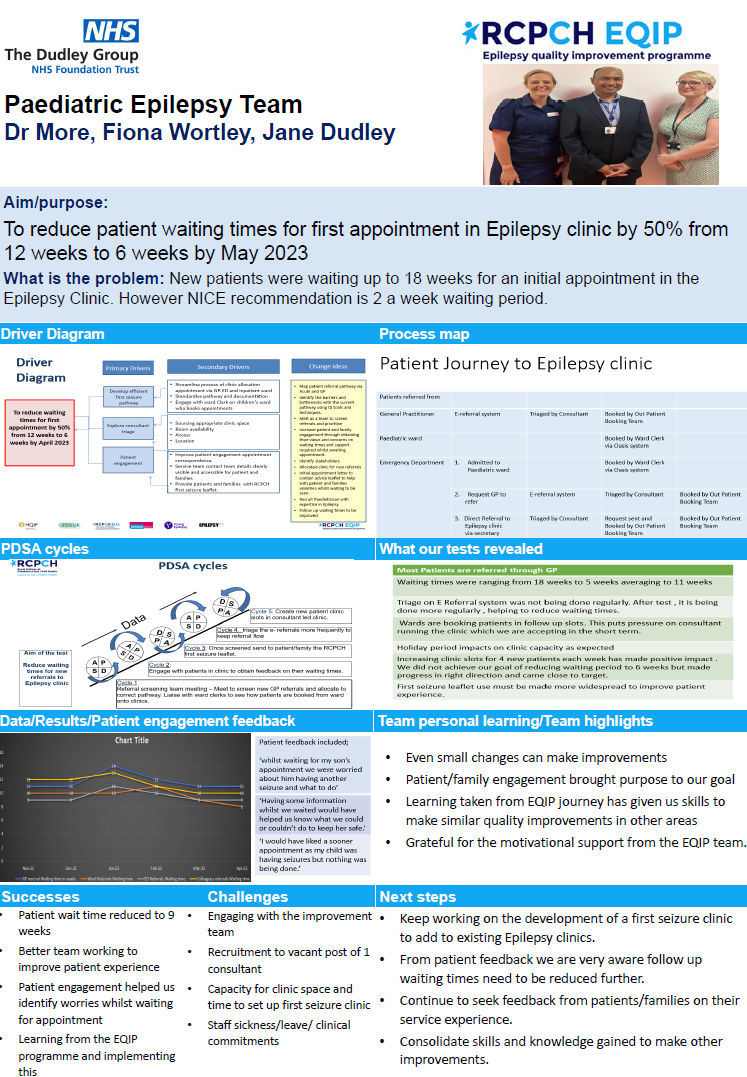
To reduce patient waiting times for first appointment in Epilepsy clinic by 50% from 12 weeks to 6 weeks by May 2023

Project aim
To reduce patient waiting times for first appointment in Epilepsy clinic by 50% from 12 weeks to 6 weeks by May 2023.
Background
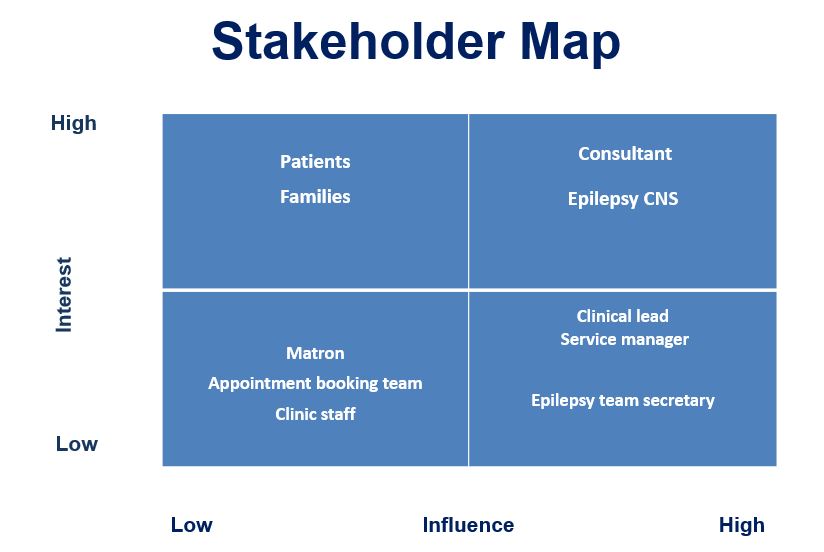
We are a paediatric epilepsy service within an acute general district hospital. The team consists of 1 x WTE consultant with specialist interest in Epilepsy and 1 x 0.9 WTE Epilepsy nurse specialist and 1 x WTE paediatric secretary. We run consultant led and nurse led clinics.
There are currently over 215 patients with a known diagnosis of epilepsy under our care. We work closely with tertiary colleagues managing children and young people with complex epilepsy. We provide advice and support to our community colleague’s including school nurses, community nurses, social services, allied health professionals, GP’s etc.
We have a transition to adult services pathway in place.
Currently working on a clinic proforma to capture all required information at new and follow up consultations. This will ensure consistency and capture data that can be easily transferred onto the epilepsy12 audit. We have developed a paediatric epilepsy report to capture the number of patients with a diagnosis of epilepsy. We are continuing to input patients into this report, but current figures are 215 with a known diagnosis.
We engage and signpost to epilepsy charities. Our transition nurse for the trust runs a youth forum and has engaged with patients with epilepsy in this forum. Listening in action and 15 steps initiatives are also utilised within paediatrics and have captured the voices of young people and families.
We would like to reduce first seizure/new referral waiting times by developing a first seizure clinic with consultant and epilepsy nurse, with an aim for patients to be seen within 2-4 weeks of referral. Our current wait time is at least over 8 weeks. This can cause huge anxiety for families especially if the child/young person is continuing to have seizures with no clear advice/support or plan for investigations/treatment.
Project planning
The teams aim is to reduce the waiting times for new patient referrals which is currently around 12 weeks. The team want to be more in line with NICE guidance but feel currently it is unattainable. Therefore, reducing waiting times to even six weeks would be a great starting point.
Currently when referrals come into to the Trusts they are classed as neurology referrals, making it difficult to confirm the exact number of patient referrals that should be received by the paediatric epilepsy service team.
Weekly/fortnightly patient allocation meetings to discuss all new referrals and triage or contact families if anything they could do whilst waiting for apt e.g seizure diary and video’s or refer for EEG whilst waiting.
Develop first seizure/New referral clinic.
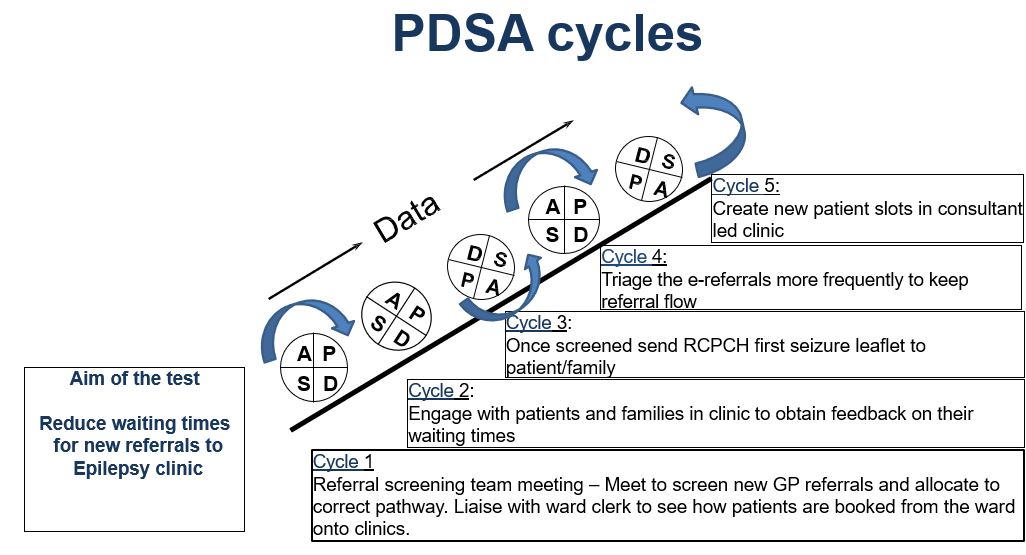
Tests, changes and what was learned in the process
November 2022
The team confirmed that patients who are referred from the GP are waiting longer because of bottlenecks then those patients who are booked from the ward that seem to find a way to get these patients seen sooner but it is unclear how this is achieved.
Ask patient/family feedback:
- How long did they wait for first appt and did they feel this was too long?
- What would have helped?
Next steps
- Meet to discuss idea’s as a team, how to get patient feedback.
- Meet with management team to discuss the potential ideas re allocation meeting and/or developing first seizure clinic.
January 2023
- We were very aware that new patients were waiting up to 4 months for an initial appointment in the epilepsy clinics.
- Recognised that 2 weeks is not achievable at this stage but needed to still work towards reducing our waiting times. We felt 6 weeks would be more of a realistic target.
- We are only a team of 2 (1 Consultant, 1 Nurse) so this would be a challenge to achieve given our other clinical commitments.
- Gathered data from informatics team who looked at; Consultant Led Epilepsy clinics, between 1st Feb 22 and 31st Jan 23. There were 166 attendances for new appointments with average waiting period of 12 weeks.
- Initial monitoring in clinic showed the waiting times for first appointment in epilepsy clinic was averaging 12 weeks.
- ESN has been shown the ERS referral system and how patients are screened and triaged new referrals. Discussed whether to meet regularly to triage and if applicable contact families to ask them to video or arrange initial investigations so these can be done whilst waiting for initial consultant appt.
- Emailed the Trust improvement team and had no response.
- Requested clinic coordinator to rename the clinics “Epilepsy” but Dr More still has a Neuro-disability FUP workload. Splitting the clinics could lead to longer waits.
- Emailed the information team for current data on waiting times
Next steps
- Meet as a team to map patient journey.
- Patient engagement
- Obtain more data from information team and Epilepsy 12 reports
March/May 2023
- Patients are referred to their service from the GP, inpatient paediatric ward and from consultant colleagues in the ED depart.
- Most patients are referred by the GP then the ward and thirdly, from the Ed dept.
- Patients that are referred by the GP receive a referral letter that is uploaded to the Trusts triage system. Recently the ESN has joined in triaging those referrals and begun the process of sending new patients an information leaflet and first aid management leaflets while they await their appointment.
- This process has just started and so the triage is happening more promptly. New patient are being added to slots within existing clinics.
- Service managers have been approached to create more clinic slots to increase the clinic capacity which has not yet been implemented.
- The aim is to first trial one clinic with the changes to see how it works, how it will benefit the patients. If successful, then these clinics will be set up on a more regular basis including joint availability, because that the idea is that it is a joint MDT meeting with both consultant and ESN.
- The new set up will allow the care team to see patients from the beginning of their journey, however currently struggling for physical space.
- We liaised with the governance team who were concerned of the clinical risk to patients who are experiencing long wait times. These patients are often seen out of hours by registrars and sent home with the promise that they will be seen in clinic soon which then creates anxiety when they are waiting for an appointment.
- We involved patients and their families who were being seeing for the first appointment.
- We also involved patients who were attending follow up appointments
- Consultant and nurse led clinics
- We asked them to reflect on their experience when they were waiting for their initial appointment.
- We saw most patients in face-to-face clinic and some we spoke to in telephone clinics.
We kept it simple by asking the following questions;
- How long did you wait from being referred to your first consultant appointment?
- Did you feel this wait was too long? Too short? Or just right?
- Is there anything that you feel would have helped you whilst you were waiting for your initial appointment?
Results
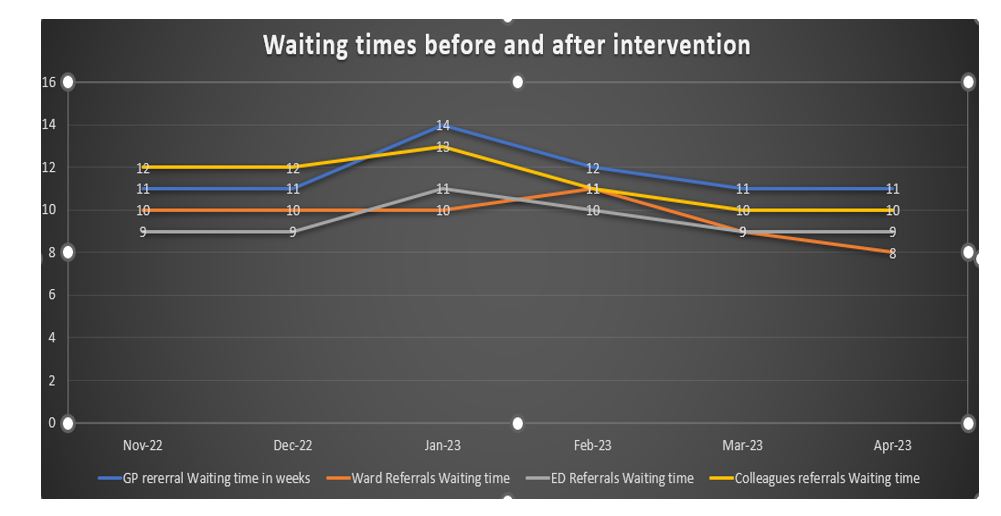
November 2022/January 2023
- Regular referral screening as a Team helped to understand the pathway and ensuring correct allocation into the most appropriate clinic.
- We learnt that doing this more frequently as a team prevented a bottleneck where patients were being referred into the service but were not being screened timely and therefore appointment allocation delayed.
- From the referral screening some health information can be sent to the appropriate patients whilst they wait to be seen in clinic.
March/May 2023
Feedback
- Most families felt the waiting time was far too long which we very much expected.
- They felt very anxious during the wait and felt they would have benefitted from more information on what to do whilst waiting for appointment. Safety, first aid, etc.
- Feedback collected on what would have had helped them while they were waiting included, most patients and families feeling concerned about what is going to happen to their child? Some were afraid their child could die whilst having a fit.
- The response received when their anxieties were reduced, were enquiring about advice on what to do in the next time it happens or is it going to happen again? Should they send their child to school.
- Patients fed back that the information contained in the RCPCH leaflet helped them to understand what they should do prior to the appointment. They said they hadn’t considered some of the safety advice in regards to baths.
- A young person said she was able to show her friends the leaflet so they could see what they would need to do to help .
- Creating new slots will make difference but we needed more clinic time to make more of an impact.
- The team are seeing eight new patients every week and collected data from them on how long they have been waiting to be seen. The results average up to 18 weeks wait time. Some have been waiting for a long time because of some miscellaneous reasons such as appointments being missed, or clinic cancelled because of annual leave or study leave.
Change
- As a result of engagement with our patients we then implemented sending them the RCPCH first seizure leaflets with the appointment letter.
- The team are considering educating the GP’s about non-epileptic disorders and developed referral pathways.
Challenges
- The Trust codes used by the booking team for all paediatric epilepsy referrals are included within neurology referrals.
- It is unclear how referrals are booked in through the EPR system or how long they are kept on from the portal before they are actioned.
- Very few patients are seen less than 12 weeks that the team can recall.
- We have really struggled to make any progress at all due to clinical commitments, sickness, engagement and motivation, small team.
- Discussed weather we could meet regularly to triage and if applicable contact families to ask them to video or arrange initial investigations so these can be done whilst waiting for initial consultant apt.
- We are currently booking at 12 weeks for Neurology.
- Emailed the improvement team and had no response. Another email sent today.
- Our clinic coordinator – We can rename the clinics “Epilepsy” but Dr More still has a big Neuro-disability FUP workload so we could split the clinics but this would lead to longer waits.
- The team have struggled to meet together to really drive the project, due to clinical commitments, sickness, engagement and motivation.
- One of the reasons for missing some of the training sessions was when we had some other clinic appointment, clinical commitment.
- We attempted to create a first seizure clinic with the clinic coordinator but no free clinic room availability.
- We did not achieve our ultimate goal of reducing waiting times to 6 weeks.
- Recruitment to vacant post of 1 consultant.
- No capacity for clinic room availability to hold the first seizure clinic and availability of both nurse and consultant.
Staff sickness/leave/ clinical commitments.
Successes
- Patient wait time reduced to 9 weeks.
- Patients and families are now provided with more safety net advice.
- Patients more prepared in clinic with diary and video’s of any seizures that have happened whilst they have been waiting. This can aid earlier diagnosis.
- Better team working to improve patient experience.
- Patient engagement helped us identify worries whilst waiting for appointment.
- Locum consultant now doing more weekly clinics which will help reduce waiting times further.
Lessons learnt
- Even small changes can make improvements.
- Things can be done in routine working hours.
- Patient/family engagement can show what the service users really needs.
- Invaluable learning taken from EQIP journey to give us the skills to make other quality improvements in other areas.
- Service has become even more patient orientated.
- This project has added to our voice of team needing more support from management.
Next steps
- Keep working on the development of a first seizure clinic to add to existing Epilepsy clinics
- Utilise ‘Hot Clinics’ on General Paediatric side to get some simpler epilepsy referrals seen sooner
- From patient feedback and our study, we know that follow up waiting times need to be reduced further
- Continue to seek feedback from patients/families on their service experience.
- Consolidate skills and knowledge gained to make other improvements.
- Share our project poster at our hospital charity funday, share success in Hospital areas
Team presentation slides and project poster
The Dudley Group NHS Foundation Trust Team presentation slides and project poster
Download to view The Dudley team presentation slides and project poster
Team presentation slides (484.0KB) Team project posters (447.7KB pdf)