South Yorkshire ICS
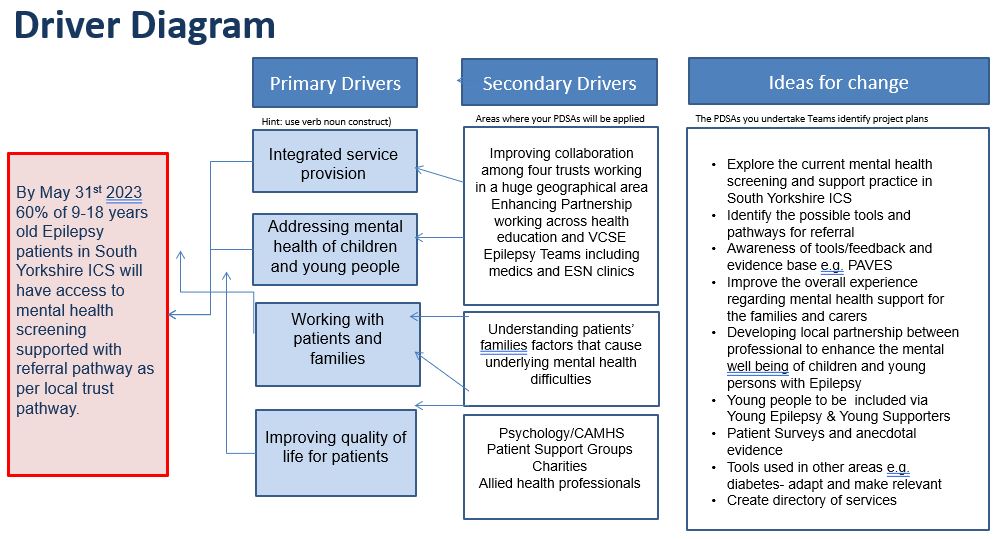
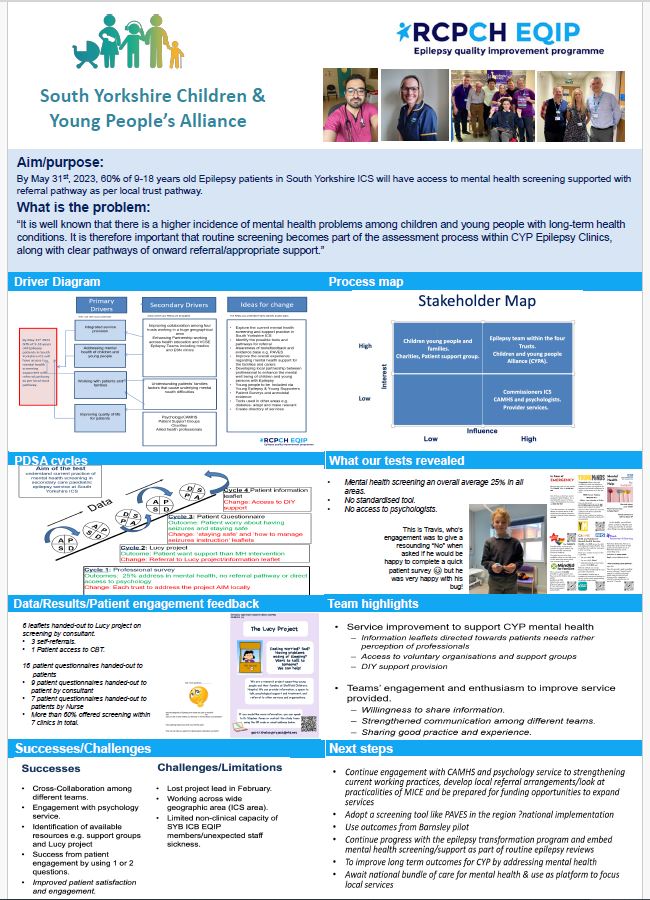
By May 31st, 2023, 60% of 9-18 years old Epilepsy patients in South Yorkshire ICS will have access to mental health screening supported with referral pathway as per local trust pathway.

Project aim
By May 31st, 2023, 60% of 9-18 years old Epilepsy patients in South Yorkshire ICS will have access to mental health screening supported with referral pathway as per local trust pathway.
Background
South Yorkshire ICS cover a large geographical area and includes three DGHs Doncaster and Bassetlaw NHSFT, Rotherham NHSFT and Barnsley NHSFT. Sheffield Children’s Hospital is our tertiary centre for Neurology, although it also provides separate Secondary Care Epilepsy Service for the City of Sheffield. The community support particularly is provided by well-established and co-ordinated Rotherham, Doncaster and South Humber NHS Foundation Trust.
The South Yorkshire ICS is a diverse team of professionals who are always keen enhance the service delivery by engaging patients and carers. Beside local QI projects, one of our major DGH partner, Doncaster and Bassetlaw NHSFT participated and completed EQIP waves twice previously. We believe that participating this current EQIP would be a fantastic opportunity to develop our regional network beside collaboration with epilepsy teams all over the United Kingdom.
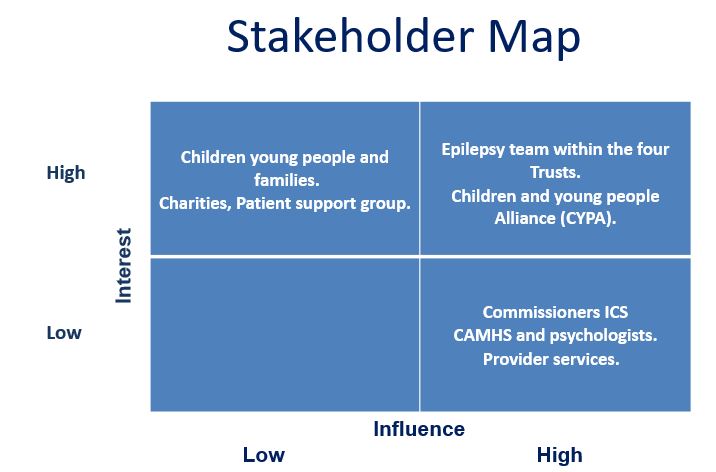
There are local and regional support groups available for patient and family engagement. We anticipate that with the implementation of ICS these groups will become more coherent and mutually beneficial.
The ICS has identified some keys areas for transformation and improvement which include,
- Mental Health Support
- Transition Services
We want to develop a mental health screen tool with the engagement of patients and cares, that can easily be utilized in clinics, both medical and nurse led. We would then aim to develop a support pathway depending up the available local and regional resources.
Project planning
The ICS consists of three District General Hospital’s and one tertiary level hospital with the neurology services. The change idea will be to initially to explore the current mental health screening and support currently available and then identify areas requiring improved tools and pathways for referral. Developing local partnerships with the healthcare professionals to enhance the mental health/well-being of the children and young persons with epilepsy.
Other areas of focus:
- Working with Improving Access to Psychological Therapies (IAPT) has raised an issue with access for patients under 18 years old who have high risk mental health conditions but do not meet the age standard for referral to
- IAPT services. Therefore, there is a need to address the problem with GP’s and local services to refer these patients that require the much-needed support from younger age groups.
- Improving upon a casual pathway by offering of better quality that can be measured via patient experience and satisfaction that a level of care is being received from local services that patients are signposted to for less complex mental health conditions. Creating a process that updates care plans and reasons for discharge from these agencies via a communication pathway that loops back to the acute service.
- Lack of clinical psychologist support for children with chronic mental illness is evident within the ICS and job role is currently vacant requiring alternative referral pathways that may not be of the same standard.
ICB management support
The focus for mental health improvement is looking at the lower tier levels of support by engaging national charities and other regional presence and have engaged with the following services:
- IAPT
- CYP voice organisations
- Psychology department based in Sheffield Children’s hospital
Anticipating the release of the bundle of care nationally, which has some overlap in focusing on improving mental health provision and should hopefully down the line feed into all work streams such as epilepsy.
As an ICB, each Trust acknowledges what the other is doing and available resource within their location and in the process of building upon it. We plan to present their improvements as a whole. We understand we don’t all have to work on the same thing but can work on components that still achieves the project aim. We plan to revisit our aim and make tweaks to some of the wording to make it more achievable for everyone, resulting in rethinking how the project will be run.
Tests, changes and what was learned in the process
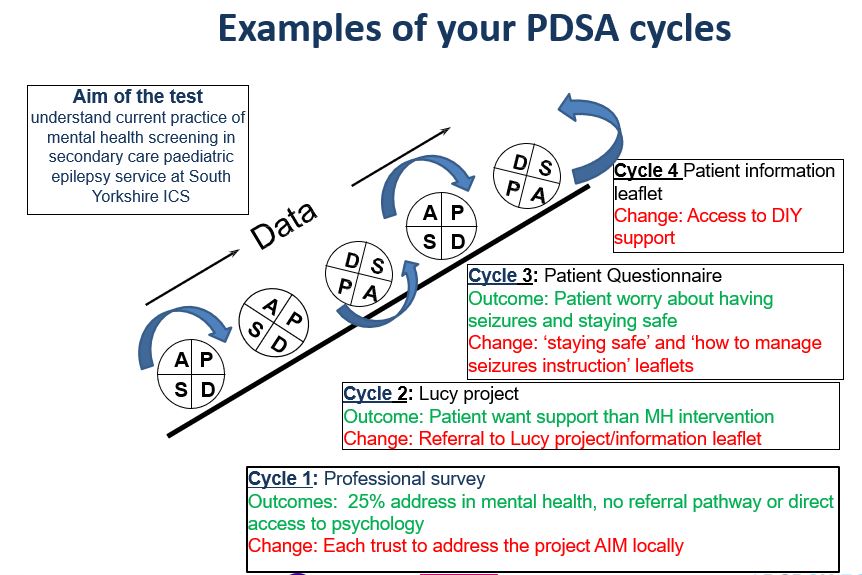
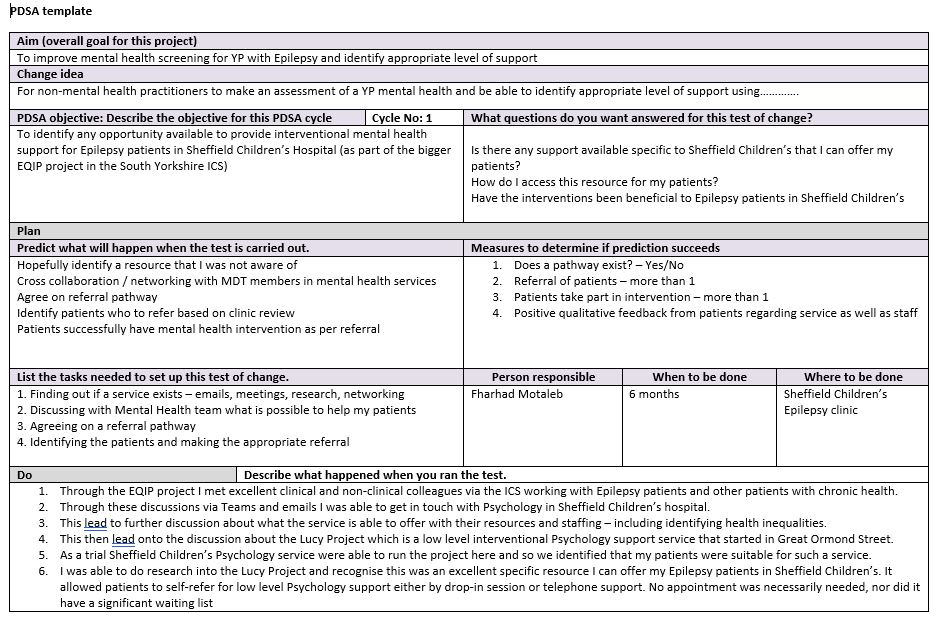
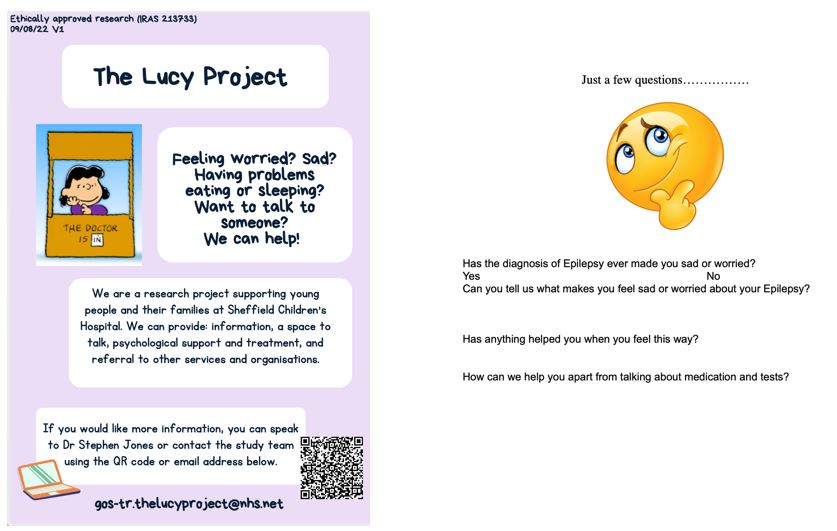
November 2022
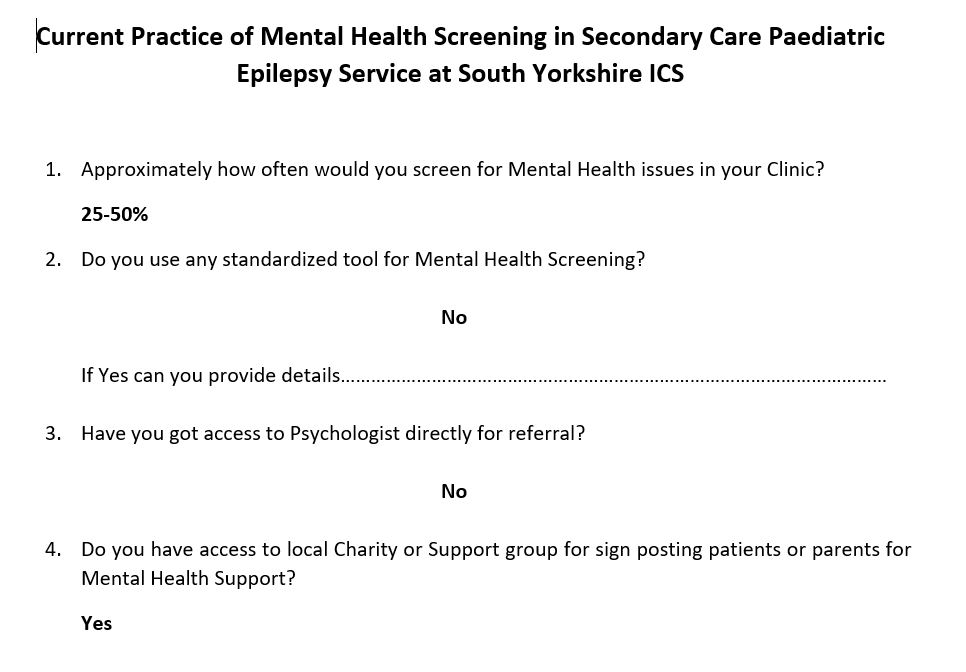
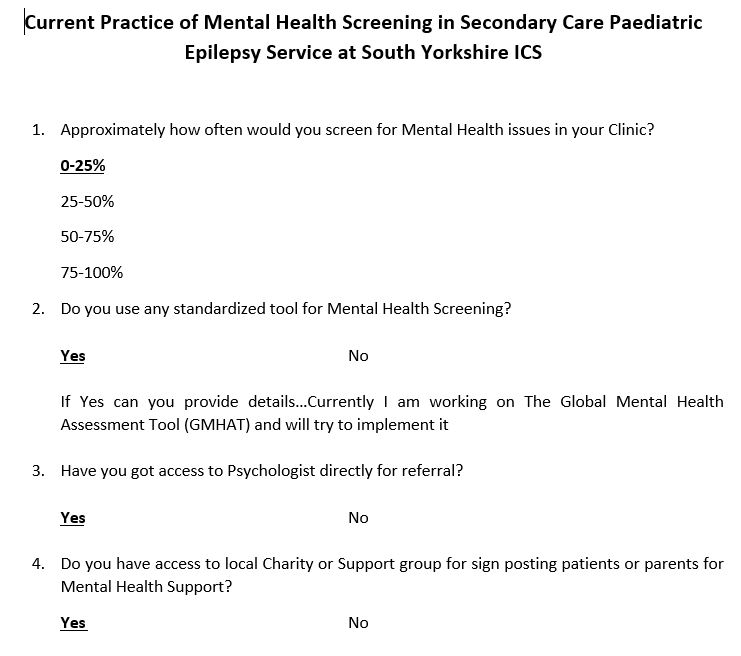
We are within the discovery stage of trying to ascertain the current processes in place from each Trust that is offered to patients for regular mental health check-ups and the standardized tools that are used. We are collecting this info via a simple survey of four questions to be filled in by their colleagues in each Trust. The questions are:
- How often would you screen for mental health?
- Do you have any standardized tool for mental health screening?
- Have you got access to psychologist directly
- Do you have access to local charity or support group for send posting parents or patients for mental health support?
January 2023
Doncaster
- Lead epilepsy consultants and nurses have completed a baseline questionnaire on current service provision for mental health. They have created a patient and family survey with baseline data that shows discrepancies of what access is available. The local team will focus on this for the next four months and then include this as part of the EQIP project. Tests will begin next week, and patients will be asked a few questions & signposted to local charities. Feedback will be requested in a month or two on their experience. Additionally, plans are in progress assess the available support with mental health screening tools.
Barnsley
- Barnsley looking to adopt Global Mental Health Assessment Tool (GMHAT) to identify number of patients that require mental health support to build a business case for mental health support offers.
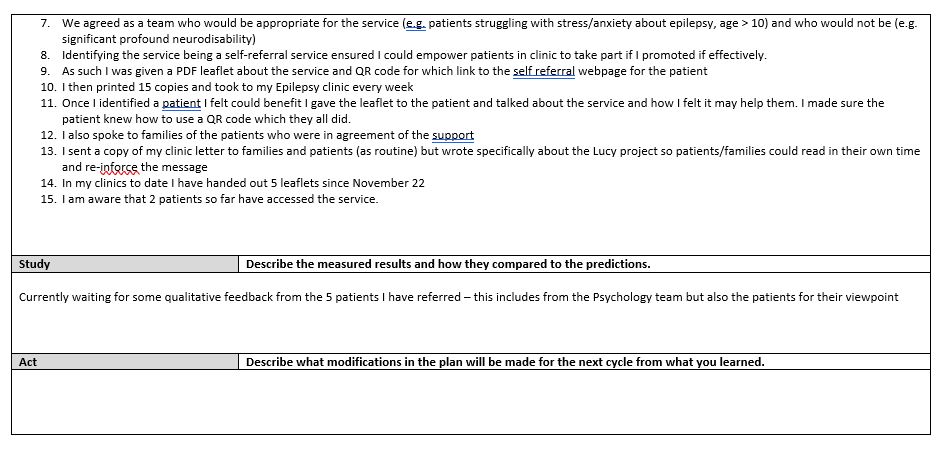
Sheffield
- Sheffield looking to scope mental health support services available to Epilepsy patients (e.g., Sheffield IAPT, SCFT Lucy Project). They have made progress in engaging a psychologist that was a part of the ‘Lucy project’ and had a helpful discussion regarding access for support with mental health for children and young people younger than 18 yrs. old. This resulted in gaining access to a pilot by the Lucy project that started in Great Ormond St which they have now utilized in Sheffield where the children can just self-refer and access low level support.
Rotherham
Are in the process of recruiting a psychologist the collating and will be engaging with patients on how they found experience of the future changes.
SYB ICB epilepsy leads met with Young Epilepsy charity’s Young Supporter who is a 20-year-old University student with Epilepsy who would be happy to engage with the Epilepsy Transformation program, including EQIP.
Chilypep has successfully been awarded the tender for CYP Voice from the SY ICB CYP Alliance to collate the views of CYP across SY to input into CYP Transformation Program workstreams, including Epilepsy.
We are unsure if patient and parent engagement takes place at SYB Trusts for Epilepsy within clinics.
Next steps
- Revisit aim and driver diagram to ensure it is realistic and achievable
- Each Trust to identify their area of focus in mental health and plan tests/patient engagement
- SYB ICB EQIP Team to agree regular progress update meetings
March/May 2023
Doncaster & Bassetlaw
- Begun engaging patients and families in particular with regards to having a screening tool which has been developed during the last 2-3 weeks. This intervention will be in place until a formal pathway has been established.
- Developed a brief questionnaire for use in clinic- possibly to be considered as a pre-screening tool/opportunity
Barnsley
- Attempting to develop an app which is a mental health assessment by mental health trained medics. Meanwhile, patients are being signposted. Looking to pilot mental health screening app for non-mental heath professionals and progressing with the Mental Health app and have discussed with some of their CYP.
- Behavioural or patients with conditions such as autism or ADHD are being supported by community services in the area which takes the load off the ASD assessment, which is associated with the elaborate mental health assessment. ADHD patients are also supported by CAMHS although there is a long waiting list.
- Building relations with a school team or school nurses to support children and young people with anxiety, stress or low self-esteem because these presentations of these conditions are not supported by CAMHS.
- In the process of making a business case for assured psychologist to support both the epilepsy and diabetes service.
Sheffield
- Conversations taking place about the patients that have been identified as needing or not needing the questionnaire,
- Identifying patients who are appropriate for the Lucy project, it’s a form of screening and will look at the wording so it does not sound too formal.
- Now engaging patients in Lucy project have engaged in a research project and have referred 5 patients- awaiting feedback and awaiting feedback
Rotherham
- Rotherham to look at referral opportunities for those that don’t reach CAMHS criteria
- Still in the process of securing a psychologist for the epilepsy team.
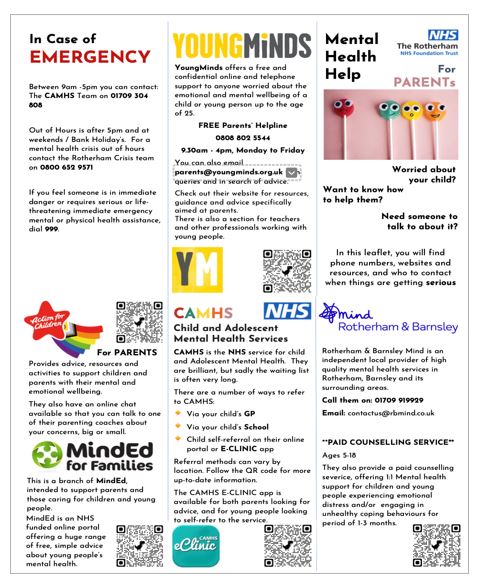
- Developed a leaflet in containing information about how to approach CAMHS.
- Attempting to develop a short tool using a few questions which is used in diabetes and implement in clinic. However, the first step is to gather the information about the available resources and design a signposting package to share with patients.
ICB support
From an ICB point of view, from the national transformation perspective we have begun to unpick the different services within different areas in the ICB that offer mental health support that previously unaware of. Resulting in approaching theses services in terms of access to psychological support or access to well-being support. EQIP has provided the team space to look for these opportunities and open those doors then spreading that knowledge to clinicians within the ICS.
- Looking at the bigger picture and there has been some funding for use of the P.A.V.E.S tool and implementation happening in the Northeast region and in other regions which will be piloted.
- The engagement box arrived, and the team reported back that the Furbies are a hit with patients. The Furbies and pens were, used in clinic.
- Patient and family have given photographic permission to use them in their project poster.
- Results from patients who has responded yes to their questionnaire had worries and anxieties. Follow up questions of ‘what are your particular worries?’ uncovered important learning from one patient wrote in I’m worried about dying because I know that patients with their epilepsy can die. This patient also indicated preferring speaking with Carys alone about this particular concern without their parents present.
- This has been a success for team in discovering so much from their patients from using one or two questions and the engagement pack.
- Another example is when a patient was worried about having a seizure in the middle of the school and worried about what will happen and felt a lot of anxiety about it. This was uncovered by simply asking how do you feel?
Next steps
- Continue with patient engagement within clinics
- Feedback from Lucy project
- Feedback from Barnsley pilot- yet to implement but have positive feedback from CYP
- Consider future implementation of PAVES tool
Results
November 2022
The ICS have received up to four survey replies so far and have agreed the next steps would be to engage and work with the patients and families to improve the experience and quality of care in this area for both the patients and the families.
January 2023
Test Outcome
- Mental health screening an overall average 25% in all areas, No standardised tool, No access to psychologists in the whole SY region
Guide to further steps
- Each trust will do separate tests
- Explore local services
- Manage local expectations
- Keep sharing experience via bimonthly meetings
- Ultimate aim for implementation of care package
March/May 2023
- Finding out what specific concerns our CYP have and how we may be able to help
- Feedback from patients in Lucy Project (Sheffield)
- Formulating a directory of services for signposting
- 6 leaflets handed-out to Lucy project on screening by consultant.
- 3 self-referrals.
- 1 Patient access to CBT.
- 16 patient questionnaires handed-out to patients
- 9 patient questionnaires handed-out to patient by consultant
- 7 patient questionnaires handed-out to patients by Nurse
- More than 60% offered screening within 7 clinics in total.
- Patient information leaflet for DIY support and introduction of questionnaire
- Development of questionnaire App
Challenges
- Increasing and improve the communication between the ICS Trusts service epilepsy teams
- Methods to capture and monitor project progress
- Overlapping areas between the work of the epilepsy transformation which is dictated by the national priorities and the EQIP.
- Increased ESN involvement
- Support from CAMHS team and different support groups or charities which are available.
- There are services that already exist, but it is difficult making the link to these services to support their children & young people needs.
- The ICS project manager is leaving the team.
- Change in EQIP leadership and approach
- Limited non-clinical capacity of SYB ICB EQIP members
- Making a business case for psychologist at Barnsley hospital Trust to support both epilepsy and diabetes
- That post is not very attractive for a psychologist role, therefore expanded the role to include more than one long term conditions, mental health support or psychology support which would be a more attractive proposition.
- The consultant at Barnsley service is concerned that the psychologist role is unclear whether they would it be an integral part of every epileptic assessment for the patient or just for selected people?
- The children and young people seen in Barnsley have more than 50% or 60 or 70 do not need that level of support, around 20% could have mental health issues, a minority of patients have severe behavioural problem or autism, or severe learning difficulties related to their epilepsy, so the second group which are having associations could be addressed by community services or by CAMHS. Therefore, the assumption is the psychologist would support the patients identified with complex needs.
- The team confirmed there would be an exclusion criteria, for example, those cases that have been already identified.
Successes
- Cross-Collaboration among different teams.
- Engagement with psychology service.
- Identification of available resources e.g. support groups and Lucy project
- Success from patient engagement by using 1 or 2 questions.
- Improved patient satisfaction and engagement.
Lessons learnt
- Service improvement to support CYP mental health
- Information leaflets directed towards patients needs rather perception of professionals
- Access to voluntary organisations and support groups
- DIY support provision
- Teams’ engagement and enthusiasm to improve service provided.
- Willingness to share information.
- Strengthened communication among different teams.
- Sharing good practice and experience.
Next steps
- Continue engagement with CAMHS and psychology service to strengthening current working practices, develop local referral arrangements/look at practicalities of MICE and be prepared for funding opportunities to expand services
- Adopt a screening tool like PAVES in the region ?national implementation
- Use outcomes from Barnsley pilot
- Continue progress with the epilepsy transformation program and embed mental health screening/support as part of routine epilepsy reviews
- To improve long term outcomes for CYP by addressing mental health
- Await national bundle of care for mental health & use as platform to focus local services
Team presentation and poster
South Yorkshire ICS team presentation and poster
Download to view South Yorkshire ICS team presentation and poster
Team presentation slides (4.2MB) Team project poster (2.3MB pdf) Sheffield PDSA example (28.8KB document)