Royal Free London NHS Foundation Trust
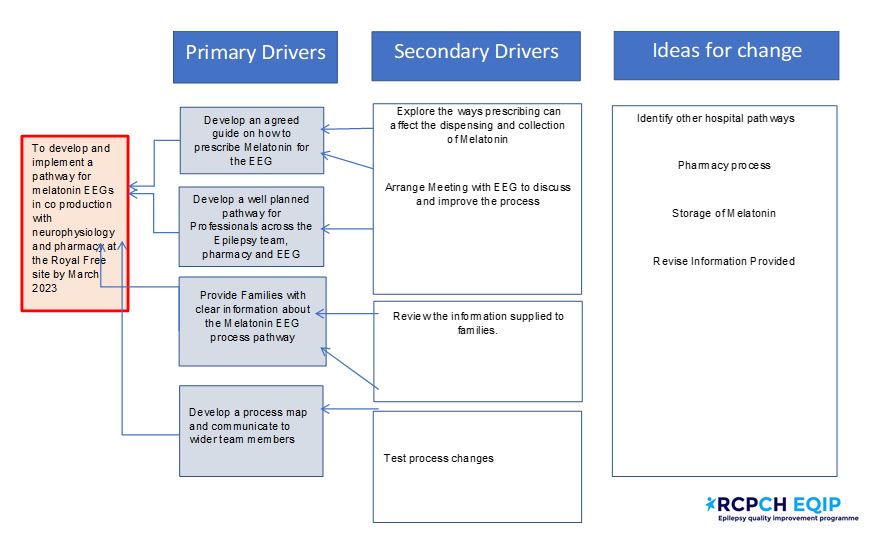
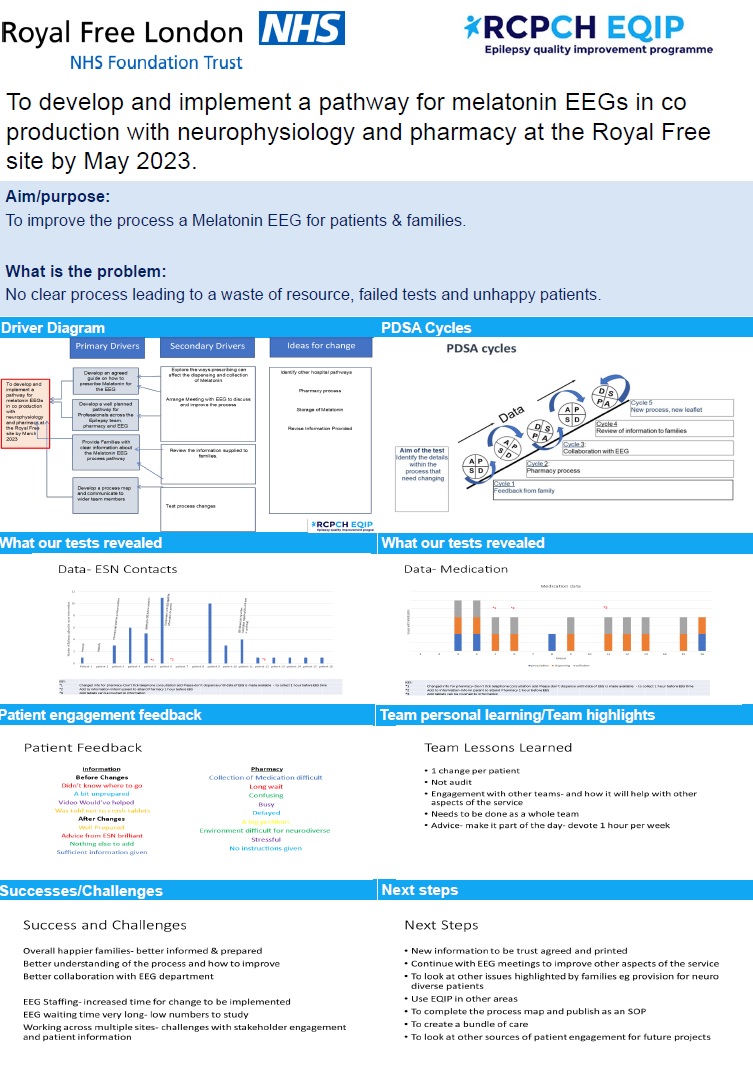
To develop and implement a pathway for melatonin EEGs in co production with neurophysiology and pharmacy at the Royal Free site by May 2023.
 |
 |
Project aim
To develop and implement a pathway for melatonin EEGs in co production with neurophysiology and pharmacy at the Royal Free site by May 2023.
Background
- 400 patients seen at 2 DGH sites under Royal Free NHS TRUST.
- 2 consultants, 1 WTE Epilepsy Nurse covering Barnet and Chase Farm hospital
- Unhappy patients, ESN Workload, Failed tests, Waste of Resource
- No clear process
- Too many variables
- Inconsistent information
- Varied prescription and dispensing
- Across 2 sites & 3 departments
Project planning
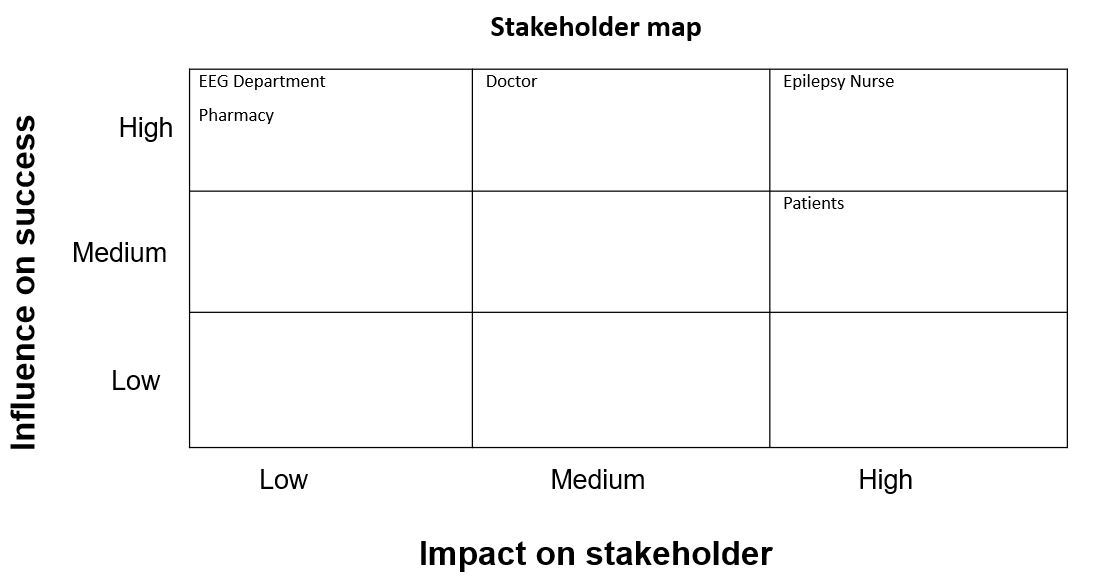
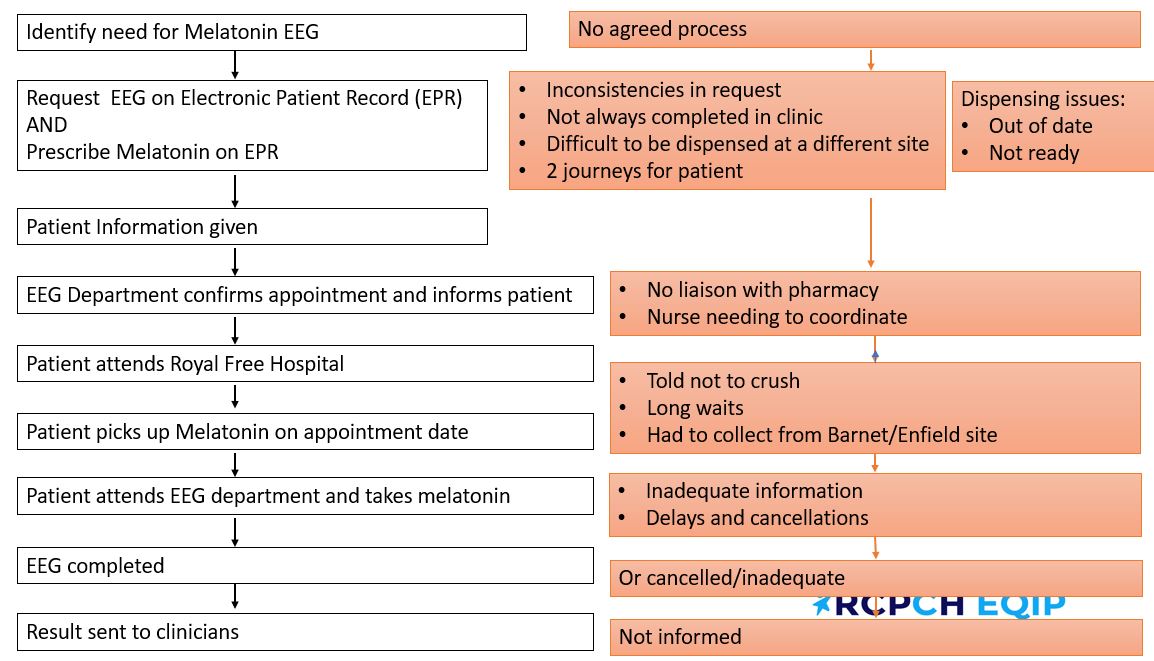
We have been working on planning our project aim and have drafted their team driver diagram and stakeholder map. We accessed the website to watch bitesize videos of diagnostics QI methodologies to begin mapping the referral pathway which involves collaborating with pharmacy and the neurophysiology department colleagues. In terms of patient engagement, we considered whether this project would be resolving the issue for healthcare professionals rather than patients and however, after some feedback received from parents/families which expressed their frustration and disappointment of the process.
Our Trust has an electronic ordering system, and we have begun looking into melatonin EEG’s that are ordered as a telephone consultation or as a face-to-face consultation? Reviewing what is written in the referral form box? Looking for similarities in the process? Engaging with the two consultants that order them within their service.
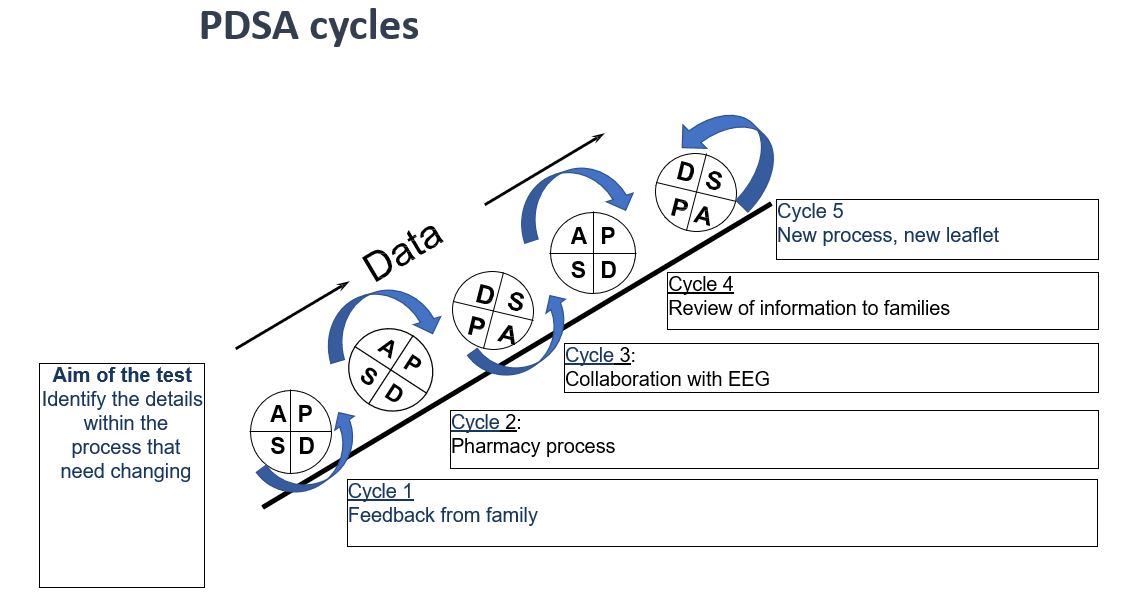
Tests, changes and what was learned in the process
November 2022/January 2023
- PDSA cycle – on all the EEGs ordered
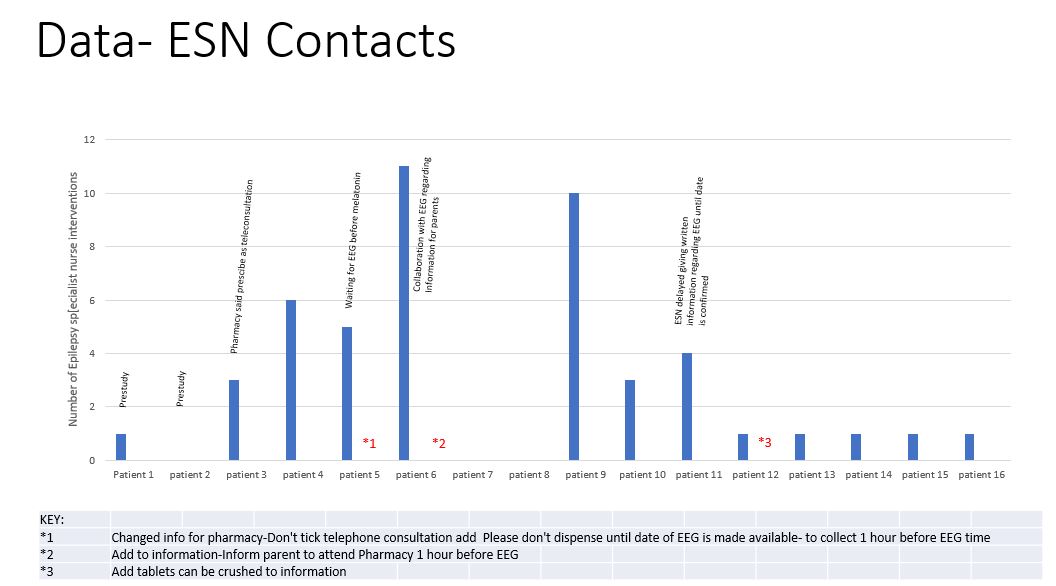
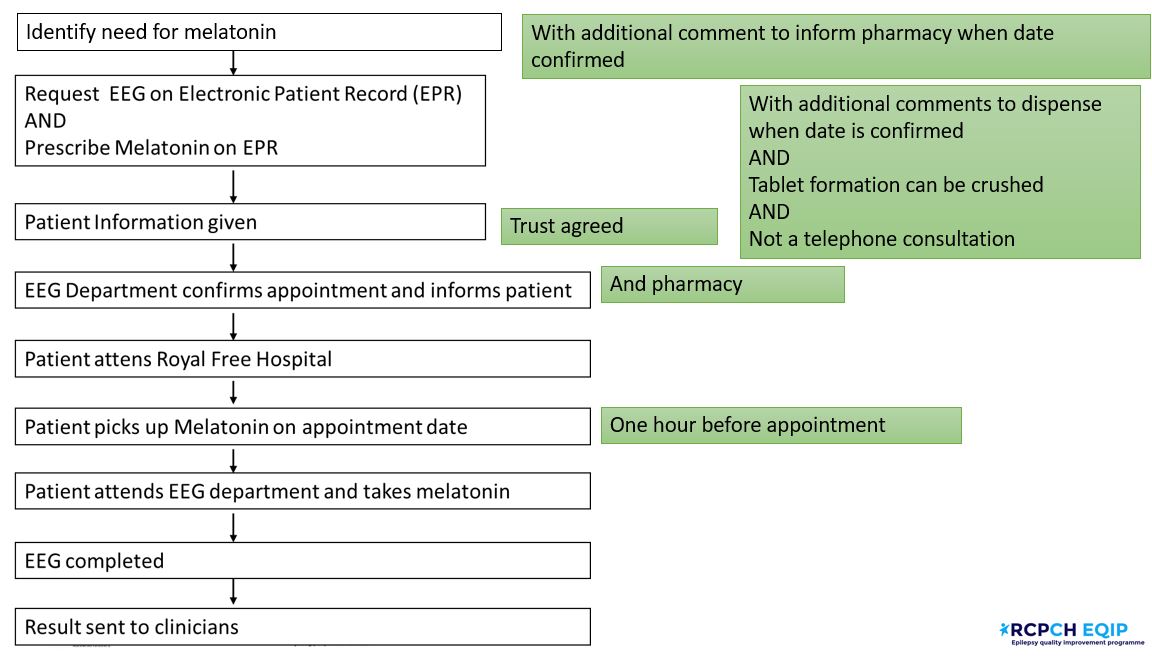
We found considerable variation in the referral pathways and decided to include the details of the pharmacy on the order form within this process to avoid relying on our ESN to follow up and chase whether the melatonin had been prescribed and the parents/carer had been informed.
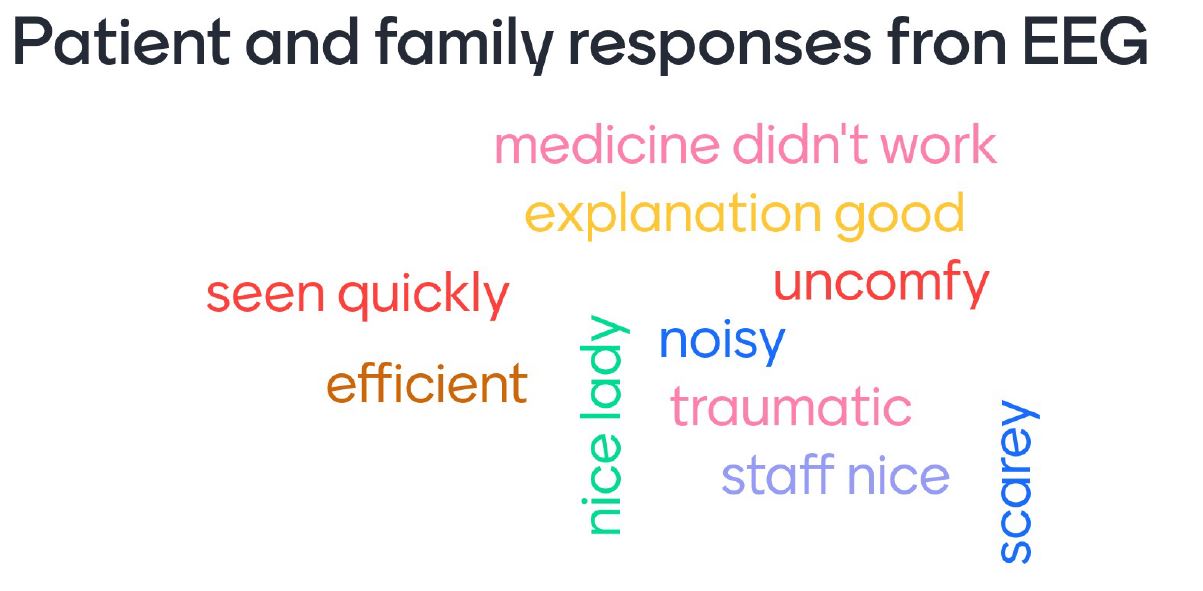
- Patient Engagement tool- to inform parent information
In terms of patient and engagement there was no clear primary drivers of the things that crash and burn our improvement project. However, if there is no pre-explanation to the patient about the system, the EEG experience is not going to be good, and if they don’t receive the medication, it will not happen.
Patient engagement tool (parent specific) has required chasing and is challenging as the test takes place on a different site- should we consider a phone interview – What would have liked to have known about the Melatonin EEG?
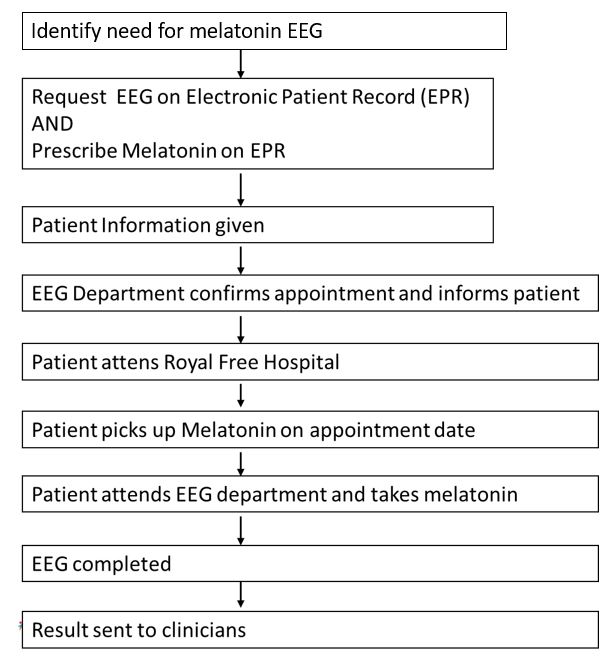
- Process Map- to inform department
Our assumptions included envisioning the project as one process but we later acknowledged it involves lots of little areas of activities going on at the same time which has provided a better understanding of QI methodology.
Next steps
- Waiting to study outcome of current orders.
- Waiting for meeting with EEG.
- Reducing the scope of the project.
- Level of engagement and input from EEG colleagues due to significant backlog they are currently experiencing.
- Choosing an effective patient engagement activity to capture feedback and views of issues to then incorporate them into project improvements.
- Identified other issues that need addressing eg collection of medication, time of EEG, challenges for neurodiverse children including environment of the EEG department, doses of melatonin, results.
March/May 2023
- PDSA cycles – on prescribing and ordering of Melatonin
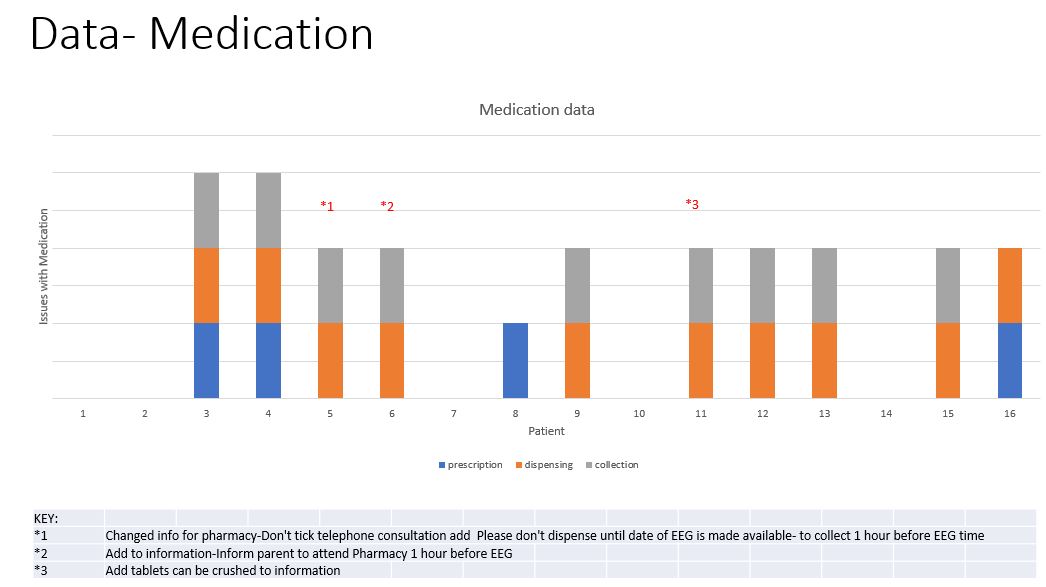
On prescribing and ordering of Melatonin are going well and the team are working their way through their patients. 14 patients have fedback they depend on how you prescribe, and the team investigated how their service prescribe when ordering the melatonin. We uncovered that the melatonin affects the end result of the patient receiving the EEG. We engaged the inhouse pharmacy to understand what the correct process should be when ordering melatonin for an EEG. The change in process by including prescription details and adding the pharmacy details on the order form was tested and we found that it’s been a great improvement.
- Patient Engagement tool- follow-up calls after EEG
We learnt that patients and families are not being told that dispensed melatonin tablets can be taken crushed for patients unable to swallow tablets. This missing guidance has resulted in EEGs being cancelled because the melatonin was not taken in time because not all patients can swallow tablets, especially for a child with Autism requiring a liquid format to take their medicine. These patients have experienced waiting an hour for the medication only for their appointment to be cancelled because they were too late in receiving the EEG. At no point along this pathway are the families informed of being able to crush the tablets.
Other issues we uncovered included:
- The sleep hasn’t been initiated,
- The environment hasn’t been suitable,
- Other areas that have been highlighted which will be raised at the next EEG meeting to resolve some of the issues and look for ways to include the patients voice going forward.
- Process Map- to inform department Process map made in draft form
When we prescribe melatonin using the new internal EPR system, we discovered if you didn’t tick a specific box, it would go to the pharmacy and be dispensed there and then. However, it’s important to know that the system moves on to the next screen page without prompting ‘Do you want the box ticked or not’. Resulting in the melatonin being prescribed earlier than the time of the EEG. The issue with this is the patient that attends the appointment will be told the EEG was out of date, therefore, we were able to identify the uncoordinated process and are currently trying to improve this pathway into a more efficient transition.

Results
November 2022/January 2023
- The data so far as informed the changes of process in ordering EEGs, prescribing, dispensing and collection of Melatonin.
- Confirmed process for Melatonin prescribing with Pharmacy- put into practice with 7 patients- result await on PDSA cycle.
- List made of the study group to monitor for outcome.
- Change of practice when requesting Melatonin EEGs – additional request on EPR- put into practice on 2 patients- results awaited.
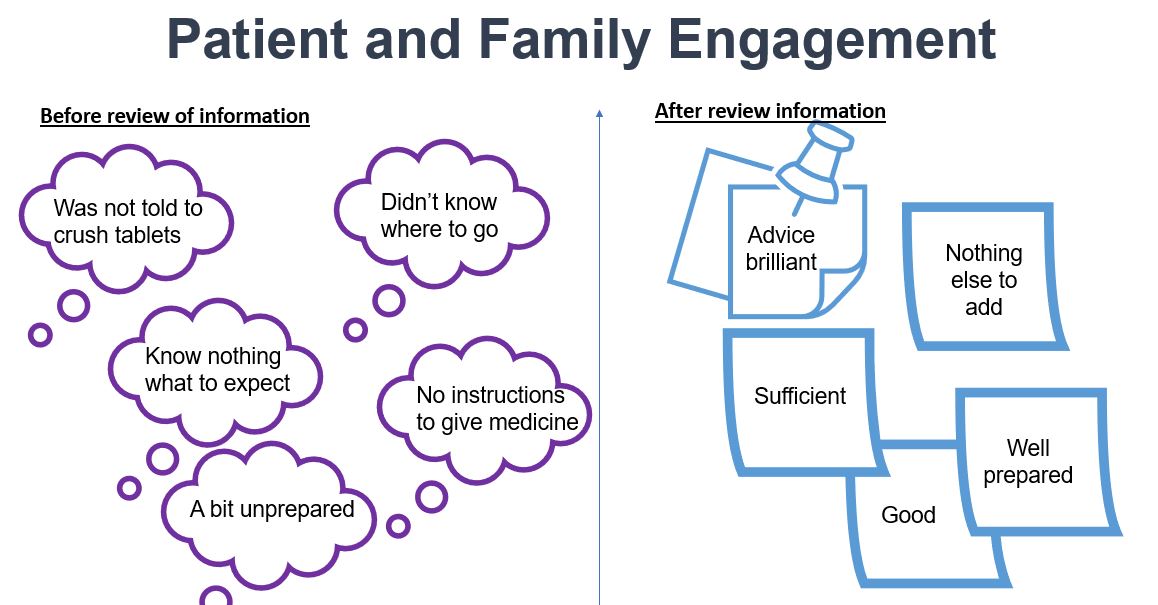
- Patient leaflet has been reviewed.
- Contacted the EEG department- asked if in use- feedback received on additional information.
- Information added
- Patient engagement tool given to 2 patients – feedback given on what would be useful to include in a leaflet- add map.
- Process map made in draft form
March/ May 2023
- 14 patients . Results for 7 patients – plan to display results on a bar chart- before and after PDSA cycles
- Results are showing changes and also highlighting new aspects
PDSA Cycle 1-Patient & Family Engagement Tool
- First 5 patients attempted questionnaire- who/ how/ change
- Engagement from 2/5 with persistence.
- Change of engagement to direct calls after test asking for feedback.
- Engagement from 5/5.
- Identification of issues-missing information- ie Map, pharmacy waits.
- Additional issues were highlighted too- environment of EEG, neurodiversity.
PDSA 2 Pharmacy process
- Agreement to prescribe on EPR system to be collected at the site of the EEG.
- Test of prescribing- by ticking a box determined when the prescription was dispensed- if it was dispensed at the time, it would then be out of date for the date of the EEG- process changed- agreement with pharmacy on details of the prescription order.
- Agreement to be available for collection 1 hour before EEG appointment.
- Lack of information to patient- parent arrived for EEG without the Melatonin, queue for medication resulted in late arrival for EEG, and EEG then cancelled- process changed. The patient engagement tool highlighted changes needed in the information.
PDSA 3 EEG Collaboration
- Discovered patient information given and what was required.
- Agreed for EEG to liaise directly with pharmacy regarding appointment date.
- Met with EEG management to increase stakeholder engagement.
- Further meeting ongoing- to discuss additional issues.
PDSA 4- Information to families
- Family feedback enabled changes in information given.
– eg confirmation that tablets can be crushed
– eg add video link
– eg map
In terms of data we have created a bar chart which shows the medication process is better, but the stakeholder map shows the involvement from the epilepsy nurses is still very high, which the team will work on to lower their involvement. We will continue to address and include related issues are that they have uncovered and share how many patients are affected by each issue.
Next steps
- Ongoing results
- Further collaboration with EEG to agree the information and produce leaflet.
Challenges
- We were unable to yet specify a cohort of patients that have melatonin EEG because the number is quite small (around 20 patients). However, if they can improve the outcomes for at least one patient, the team feel it would achieve something.
- We struggled with the feedback received from engaging children and young people due to the number of issues experienced with in all areas of the referral process, including information leaflets given to patients and families, collection of medicine, giving the medicine and the EEG itself. The team are in the process of trying to highlight each issue before beginning of the process of trying to improve them.
- The EEG department is not onsite as the same hospital as the paediatric epilepsy service therefore some of the issues experienced are the EEG is ordered at the time in the clinic by a consultant maybe over the phone, but the family is not in attendance or families in attendance have to travel to a different hospital to have the EEG done.
- Including patient engagement views in terms of devising a leaflet explaining the melatonin EEG pathway. The leaflet will also need to be agreed that with the EEG dept and approved by Trust policy process hopefully by April.
Successes
- Overall happier families- better informed & prepared.
- Better understanding of the process and how to improve.
- Better collaboration with EEG department.
Lessons learnt
- Start with 1 change per patient
- QI is not an audit
- Engagement with other teams- and how it will help with other aspects of the service
- QI needs to be done as a whole team
- Advice- make it part of the day- devote 1 hour per week
Next steps
- New information to be trust agreed and printed
- Continue with EEG meetings to improve other aspects of the service
- To look at other issues highlighted by families eg provision for neuro diverse patients
- Use EQIP in other areas
- To complete the process map and publish as an SOP
- To create a bundle of care
- To look at other sources of patient engagement for future projects
Team presentation and project poster
Royal Free London NHS Foundation Trust team presentations and project posters
Download to view Royal Free team presentation slides and poster
Team presentation slides (4.3MB) Team project poster (407.4KB pdf)